Beware of Poor Breast Thermograms
James S. Campbell, MD
ILSI Thermography Service
19 Sep 2012
Clinical thermography for breast cancer detection is just now being introduced into mainstream medicine, but unfortunately not every thermographer is using the best technology and technique. Even FDA-registered thermal systems may give very poor images.
Here at the Thermography Service of Integrative Life Solutions I often see thermograms done in other clinics that are of extremely poor quality. Some thermography systems that have been marketed around the USA are simply inadequate to detect breast cancer reliably. They either have poor image resolution (not enough pixels of the breast in the image) or poor thermal resolution (not enough color differentiation to detect small thermal differences). Some images have been so poor as to be non-diagnostic. You can tell a human is standing there, but not much more. This is simply not acceptable in the important field of breast cancer detection. Obviously you want the best, highest resolution image to find any problem at the earliest time.
I am also very concerned about thermographic reports that do not include the images. A long-winded report dictated by an “expert” is only as accurate as the images seen by that interpreter. Without the images, the report may be meaningless to compare with future thermograms. Because thermographic images of a person should remain fairly stable though the years, it is important for people to save copies of their images, either in print or digitally, for comparison over time. Insist on getting a copy of your images, either digitally or in print.
Another alarming thing I hear from people who have had thermography done at other sites is that they were not cooled down before the images were taken, or a modesty drape was put over their breasts during cool-down! These area grave errors on the part of that thermographer. The thermogram of a warm person does not show whether arteriolar constriction is taking place properly, and any drape over the breasts distorts the final thermal image. Arteriolar constriction (or lack of it) is absolutely necessary for the detection of breast cancer, body inflammation, infection, and circulatory changes. Thus an un-cooled thermogram for breast cancer is not reliable at all, and the woman’s money and time are wasted and her future health is put in jeopardy by such an inadequate exam.
A third problem with many thermography exams for breast cancer screening is that the underside of the breast is not imaged. If a woman with a B-sized cup size or greater is cooled down in a standing or sitting position, the underside of the breast naturally folds down against the chest wall. This prevents the underside of the breast from cooling, and a cancer in the lower portion of the breast will not be detected. Some thermographers have the woman pull up on the upper breasts to image the underside of the breasts, but this is useless unless the underside has been properly exposed to air during the cool-down process. The only really effective way to cool the underside of the breasts is to have the woman lie down on her back with arms away from her sides during the cool-down period. Then the first image is taken of the undersides before the woman stands up for the remainder of the images.
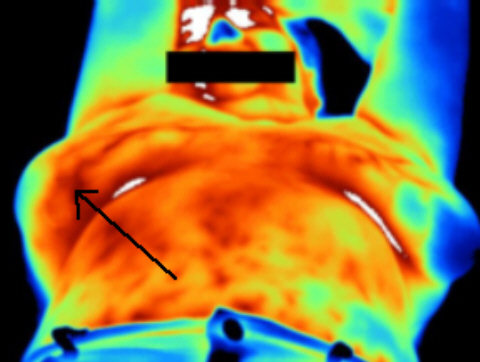
How important is the imaging of the underside of both breasts? This Figure shows a problem with the underside of this woman’s right breast. All the other images were normal. Because of this image, the woman underwent biopsy and removal of an early breast cancer that would have been missed by “standard” thermography without the supine view demonstrated here. In my experience at the Thermography Service, we have seen three such cases to date. Thus it is important to seek a thermographer who does a really complete image series such as shown in figure 3. This is our standard protocol here at ILSI Thermography Service, and we encourage all thermographers to provide similar complete and high-quality breast thermograms for their clients.
So beware of poor thermograms! Until standardization and accrediting of Clinical Thermography comes about, it is up to the patient to be sure that the procedure is done right and the images taken are the best quality. For complete diagnostic breast screening, be sure you are cooled properly. Most studies advise cooling unclothed from the waist up at 68-70F for 15 minutes before breast images are taken. For most women, lying down on her back with the arms away from the sides is best for cool-down. The first image is taken in this position, then the woman stands up for the other images, which should include a full frontal view, a close-up of each breast, the inner and outer surfaces of both breasts, and an image of the face to detect fever or inadequate cool-down (see figure 3). These images are best taken in the cool room with a hand-held infrared camera, not a stationary “camera-on-a-stick” as used by many commercial systems. Hand-held cameras are the best at this time for obtaining the close-up, underside, and oblique views needed for a good diagnostic breast thermogram.
Figure 3: Recommended Views for Diagnostic Clinical Breast Thermography